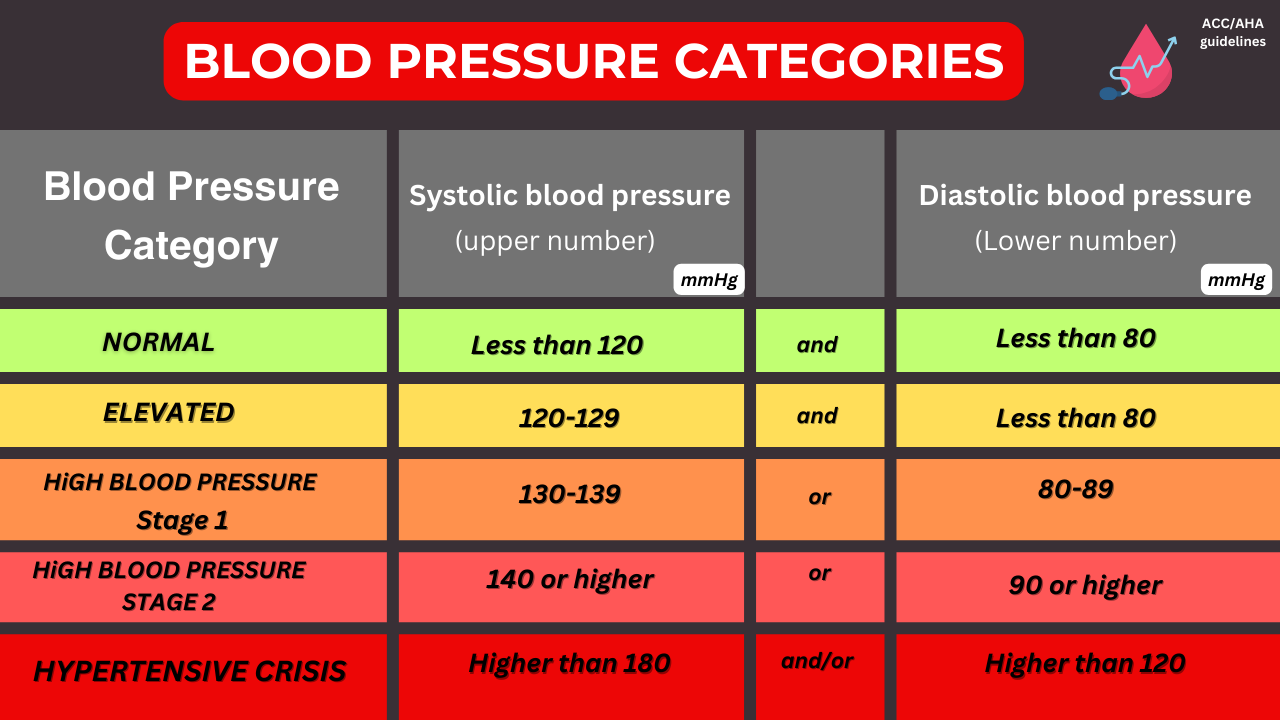
High blood pressure, also known as hypertension, is often dubbed the “silent killer” because it typically doesn’t present noticeable symptoms until it leads to more serious health complications. High blood pressure can affect your brain your heart your kidneys and other organs.
Can high blood pressure affect your skin?
We will discuss in the article below:
The Link Between High Blood Pressure and Skin Health
High blood pressure occurs when the force of blood against the walls of your arteries is consistently too high, which can lead to damage over time. This damage can impair blood flow throughout the body, including to the skin. Good blood flow is essential for delivering nutrients and oxygen while removing waste products, all vital for maintaining skin health.
Common Skin Changes Associated with High Blood Pressure
- Changes in Skin Color: Early signs of high blood pressure affecting your skin may include changes in color. Poor circulation caused by damaged blood vessels can make the skin look dull or slightly blue, particularly noticeable in extremities like fingers and toes, due to reduced oxygen supply.
- Spider Veins: These small, expanded blood vessels can appear close to the skin’s surface, often resembling red or purple sunbursts or web patterns, usually on the face or legs. Spider veins can be exacerbated by the increased pressure within the veins due to high blood pressure.
- Flushing and Redness: High blood pressure can cause episodes where the skin turns red due to dilated blood vessels attempting to lower blood pressure. This flushing typically occurs on the face and can be triggered by stress, hot drinks, or alcohol.
- Slow Healing of Skin Wounds: If you have high blood pressure, you might notice that skin injuries such as cuts or scrapes take longer to heal. This is due to decreased blood flow to the injured area, which reduces the oxygen and nutrients available for repair.
- Dry, Itchy Skin: A reduction in blood flow can also impair the skin’s ability to retain moisture, leading to dryness and itchiness. When the skin is dry, it can become flaky, rough, and more prone to irritation.

I won’t go too much into the science but the main thing you have to know are three factors high blood pressure can cause vascular damage, inflammation as well as hormonal imbalances all of these effect the skin and contribute to poorer skin health.
Skin Changes in Individuals with Dark Skin
In darker-skinned individuals, manifestations of high blood pressure may be less noticeable or appear differently: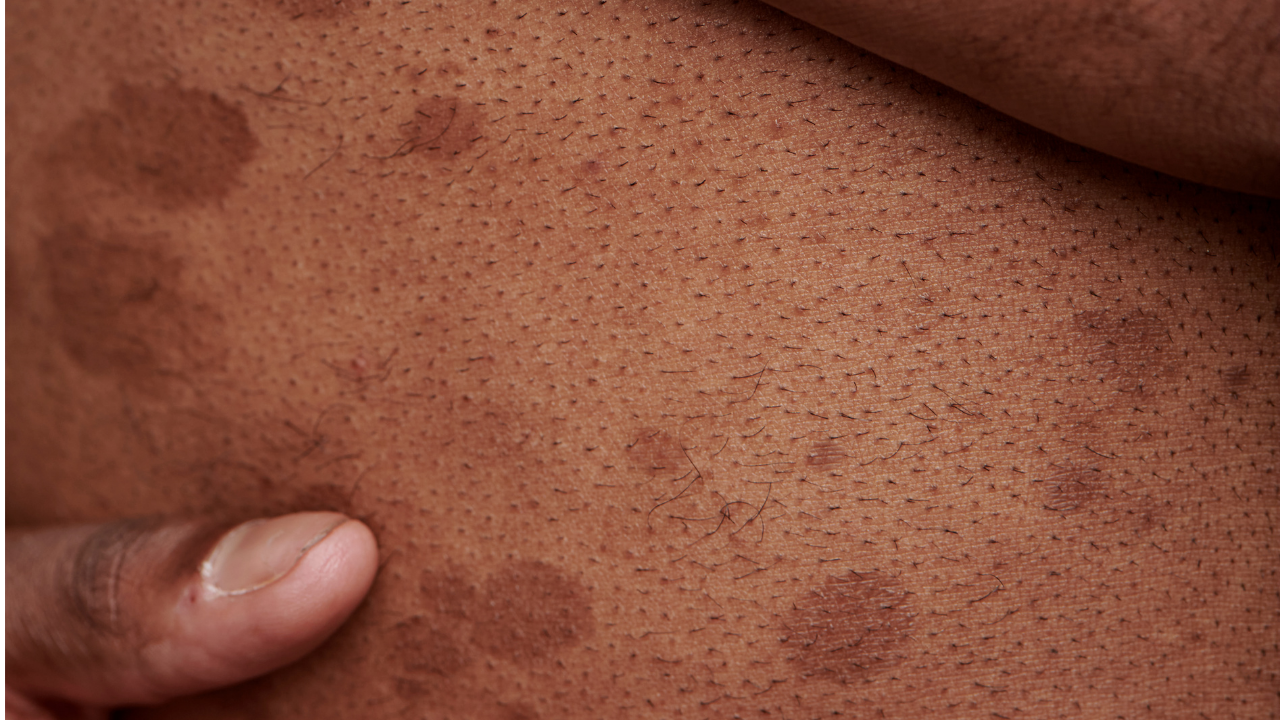
- Color Changes: Hyperpigmentation or hypopigmentation may occur, where patches of skin become lighter or darker than surrounding areas.
- Spider Veins: These may appear as dark blotches or subtle discolorations, making them more challenging to detect.
- Flushing: Less visible on darker skin; instead, the skin may feel warmer or appear shinier or swollen without an evident red flush.
- Hyperpigmentation: Prolonged damage from high blood pressure can lead to areas of the skin becoming darker, a reaction more common in darker skin tones.*(see below)
- Scarring: Delays in wound healing due to high blood pressure can lead to more pronounced scarring in individuals with dark skin, sometimes resulting in keloids or hypertrophic scars.
*Hypertension (HTN) itself does not directly cause hyperpigmentation, but certain factors associated with high blood pressure and its treatment can contribute to skin discoloration, especially in dark-skinned individuals. Here are some potential mechanisms:
-
Medication-Induced Hyperpigmentation – Some antihypertensive drugs can cause skin pigmentation changes:
- Calcium channel blockers (e.g., amlodipine, diltiazem, nifedipine) – Can cause dark patches or a bluish-gray discoloration, especially in sun-exposed areas.
- Hydrochlorothiazide (HCTZ) – Can increase sensitivity to the sun, leading to hyperpigmentation.
- Beta-blockers (e.g., propranolol) – Rarely associated with hyperpigmentation, particularly on the face and mucous membranes.
-
Chronic Venous Insufficiency & Stasis Dermatitis – Uncontrolled hypertension can contribute to poor circulation in the legs, leading to hemosiderin deposition and brownish skin discoloration.

-
Acanthosis Nigricans – Although more common with insulin resistance and obesity, acanthosis nigricans (dark, velvety skin changes in body folds) can be seen in metabolic syndrome, which is often associated with hypertension.
-
Post-inflammatory Hyperpigmentation (PIH) – Individuals with dark skin tones are more prone to hyperpigmentation after inflammation or injury. If hypertension leads to skin conditions like eczema, venous ulcers, or irritation from medications, it can result in lingering dark patches.
-
Livedo Reticularis – In severe cases of high blood pressure affecting blood flow, a net-like bluish or purplish discoloration may occur due to vascular changes.